Blepharospasm - Treatment
What is Blepharopasm?
- Blepharospasm is a nagging disorder of the eyelids that has found no cure to date despite being recognized as a disease since the 16th century and despite concerted efforts to find a viable cure. The disease is usually indolent but can progress dramatically despite treatment making the patient frustrated. This is dangerous as the patient seeks to find some relief through unconventional remedies that might be even more harmful than the disease itself.
- History reveals that people in past labelled patients with blepharospasm as being mentally unsound and were institutionalized. The treatment given in those days often resulted in serious complications such as loss of facial expression and movements, functional and cosmetic deformities of ptosis, and eyelid malposition, which were often as bad as the disease itself. This was disheartening for the patients.
- Despite the absence of a cure for blepharospasm, newer advancements in its management have resulted in fewer side effects and significant reduction in severity of the condition with functional improvement.
Treatment Options for Blepharospasm
- Patient education, membership in various support groups, pharmacotherapy, botulinum toxin injections, and surgical intervention constitute the best conventional treatments for a patient with blepharospasm. Various unconventional remedies that have found takers include faith healing, herbal treatment, hypnosis and acupuncture.
- In reflex blepharospasm, the causative disease should be treated to prevent recurrences.
General Management of Blepharopspasm
- Blocking or reducing sensory stimulation constitutes the originally line of management of a patient with blepharospasm. Wearing tinted sunglasses with ultraviolet blocking to decrease painful light sensitivity called photo-oculodynia is a simple yet effective measure. Improved light sensitivity, blink frequency, and functional limitations is noted with grey and FL-41 tinted lenses.
- Irritation of the eyes, dry eyes and blepharitis associated with blepharospasm are ameliorated by lid hygiene, frequent application of artificial tears and occlusion of the punctum.
Medical Treatment of Benign Essential Blepharospasm
- The objective of medical treatment are to reduce morbidity, possibly to halt progress, and to prevent complications. Pharmacotherapy however provides little to no relief for most patients with blepharospasm. Results with various pharmacologic agents are erratic and variable providing only marginal or transient relief of symptoms.
- Tricyclic antidepressants provide symptomatic relief by treating the underlying depression that worsens the symptoms of blepharospasm. Lorazepam, clonazepam and Artane have been used with variable efficacy.
- The most effective treatment of choice for achieving early yet temporary relief of symptoms is Botulinum toxin A with over 95% patients reporting significant improvement.
- The toxin acts by interfering with acetylcholine release from nerve terminals, causing temporary paralysis of the associated muscles. After injection, Botulinum toxin A produces peak effect after 5 to 7 days and provides pain relief as early as 2 days and lasts for up to 3 months.
- Complications of botulinum toxin injections are ptosis, corneal exposure, dry eye symptoms, entropion, ectropion, photophobia, diplopia, ecchymosis and lower facial weakness.
- Failure of Botox or Xeomin therapy is due to eyelid malposition, aesthetic concerns, apraxia of eyelid opening, or photo-oculodynia. These conditions deserve surgical intervention.
- It is commercially available in two forms - onabotulinumtoxinA (Botox) and incobotulinumtoxinA (Xeomin).

Surgical Treatment of Benign Essential Blepharospasm
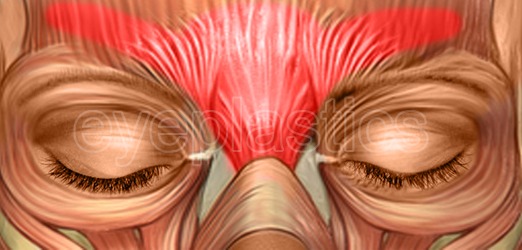
Surgical treatment is considered only when there is poor response to a completed trial of Botox Injections. Spasm of the orbicularis oculi is best treated with myectomy. Frontalis suspension and limited myectomy with complete removal of the pretarsal orbicularis is preferred for patients who are visually disabled by apraxia of eyelid opening.
1. Myectomy
Myectomy is done in stages starting with upper eyelid surgery, followed by the lower eyelid surgery if symptoms persist. Chronic lymphedema is a common complication of simultaneous upper and lower eyelid myectomy, hence it is avoided. Myectomy might be limited myectomy or extended myectomy.
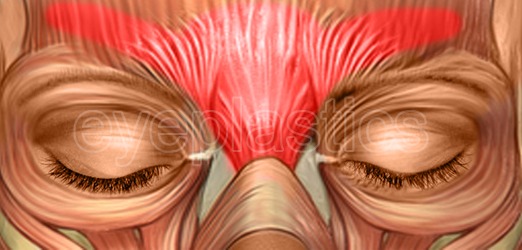
Limited myectomy: Consists of surgical extirpation of eyelid protactors, including pretarsal, preseptal, and orbital portions of orbicularis oculi muscle.
Extended myectomy: In adds to to the above, it involves removal of the procerus and corrugator muscles.
2. Superior Cervical Ganglion Block
For patients who complain of debilitating light sensitivity (photo-oculodynia) intervention by a pain clinic might be beneficial to the patient. Superior cervical ganglion blocks reduce photo-oculodynia by chemical denervation of the orbital sympathetics, thus numbing the afferent loop of the disease and providing symptom relief.
What is botulinum toxin A?
-
It is a toxin produced by the bacteria Clostridium botulinum which weakens muscles by blocking nerve impulses transmitted from the nerve endings of the muscles.
Is botulinum toxin A safe?
-
How long does it take to work?